GROUNDSWELL
Developing a restorative care initiative for oncology staff
ROLE
–
Experience Design
Project Coordinator
Product Strategy
Service Strategy
Stakeholder Coordination
TEAM
–
Lorin Anderberg
Kristin Hughes
Greg Baltus
Robertus Shuyo
Kelly McDowell
and more…
TOOLS
–
Figma
Illustrator
InDesign
CAD

CONTEXT
Groundswell is an ecosystem of support created for gynecologic staff at UPMC Magee-Womens Hospital
Beginning as a graduate-level course pitch, Groundswell includes four touchpoints: redesigned patient death notifications, guided restorative resources, a restorative pod, and a community art wall.
I co-led the project from concept to implementation. While I contributed to all components, this case study will focus on the Groundswell Pod—developing its concept, supporting production, and guiding user testing to ensure it met both emotional and operational needs.
PROBLEM SPACE
Oncology staff experience constant emotional strain burnout despite existing support structures
Informal, bottom-up coping practices often operate outside of daily workflows, revealing an opportunity to integrate emotional well-being practices into the care experience itself.

SOLUTION PREVIEW
The Groundswell Pod is a dedicated restorative space for oncology staff to pause, reflect, and recharge

RESEARCH
Through shadowing, interviews, and participatory workshops, we found that emotional processing is often unsupported in oncology care
UPMC staff described carrying cumulative emotional weight without time, language, or spaces to reflect. These insights revealed a critical gap in how healthcare systems support their own caregivers.

Through affinity mapping, we found opportunities to embed care through language, space, and ritual
Mapping these insights made visible where design could strengthen restoration within daily workflows, inspiring our initial concept for Groundswell. The pod sprouted from our second insight.

STAKEHOLDER COORDINATION
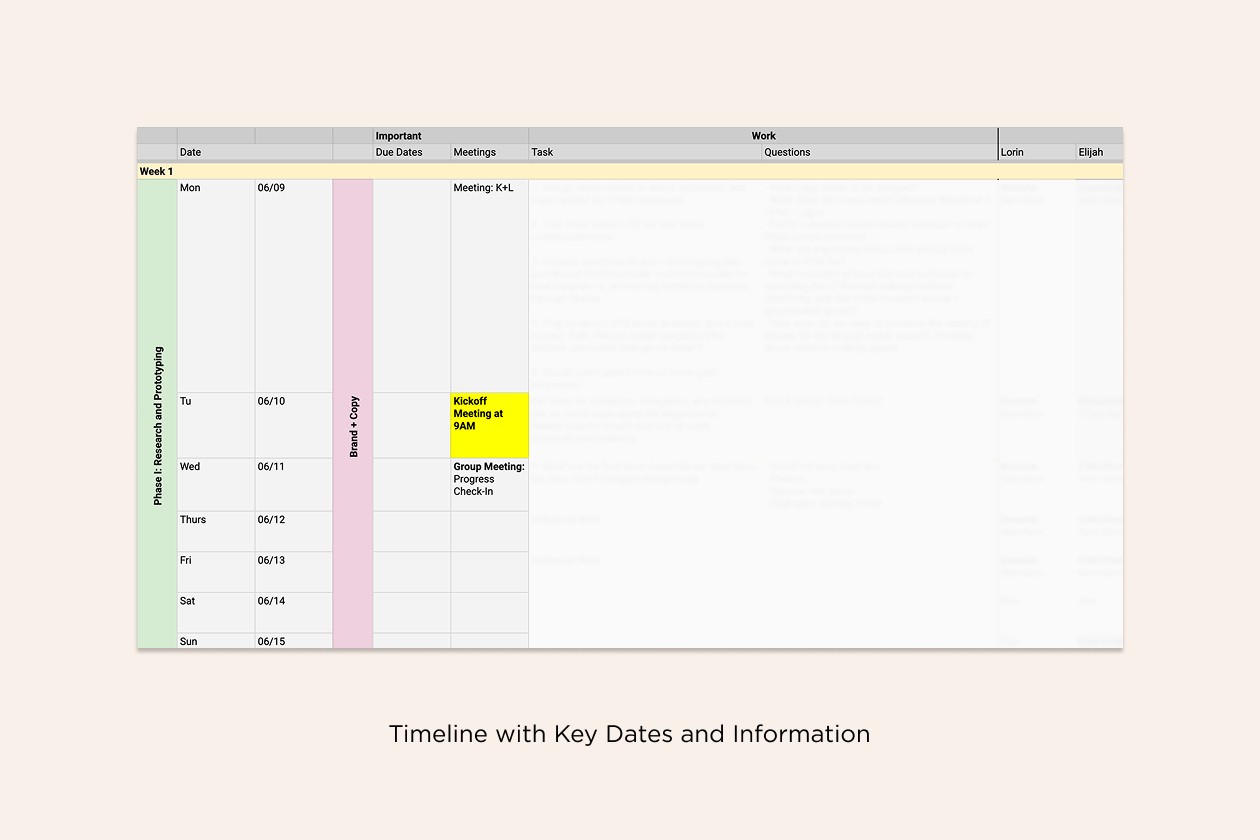
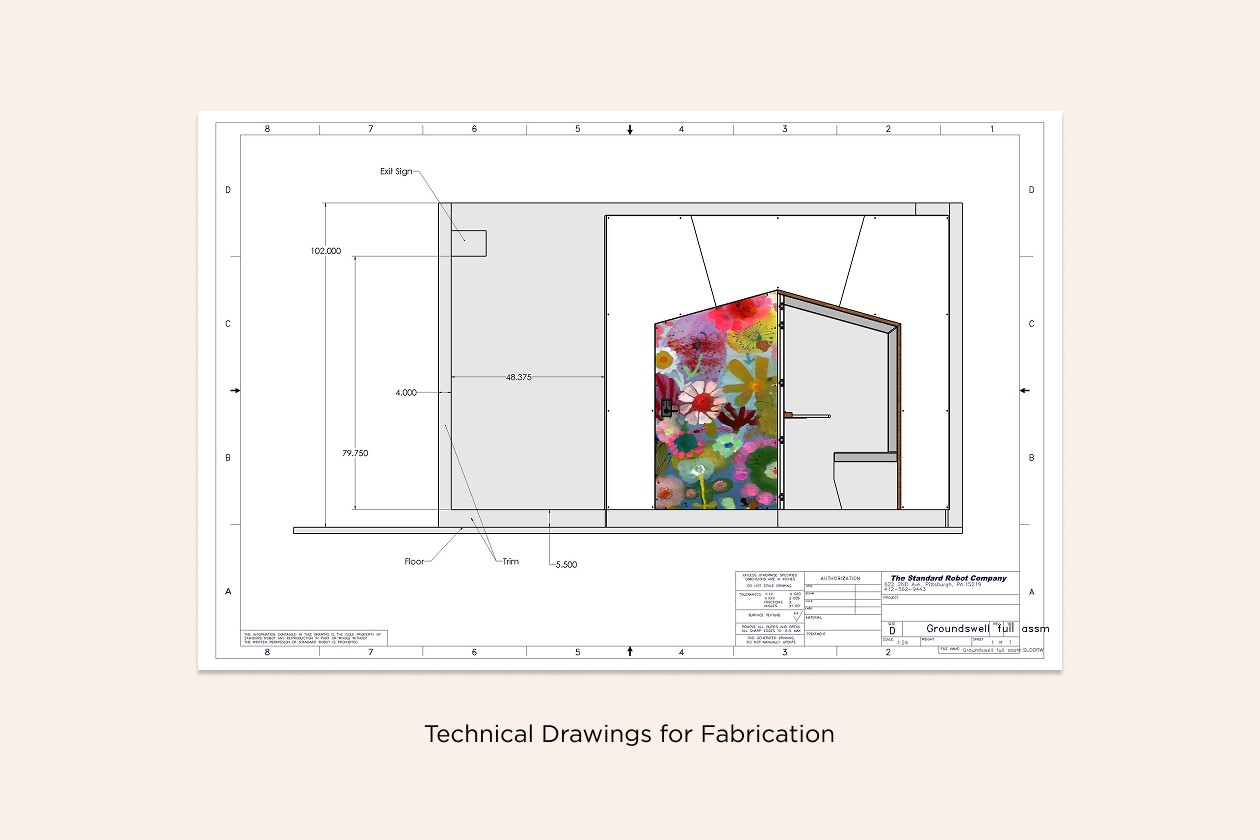
To move from concept to reality, we kept close coordination across hospital staff, hospital administration, and design and fabrication partners
Tailored communication strategies supported timely feedback, smooth approvals, and precise construction while keeping the project aligned with hospital requirements and on schedule.
KEY ITERATIONS
Designing the Pod required balancing emotional intent with hospital constraints and stakeholder needs
[1] Pod Location
Working closely with hospital administration and operations, we explored multiple spaces to find a location convenient for all oncology departments. We settled on a nook where old telephone booths had once been, adapting the building’s structure.

[2] Exterior and Privacy
Administration emphasized that the Pod remains a sacred, intentional space for Women’s Cancer Services staff. They also wanted us to add doors. We embraced these constraints, letting them guide us to create a sense of care within the hospital environment.

[3] Interior Experiences
Administration emphasized that the Pod must be respected as a restorative space and used only only for a maximum 10 minutes. We designed the interior to guide users gently, including subtle cues to help staff manage short breaks while maintaining the space’s sacred, restorative purpose.

FINAL SOLUTION
[1] Sacred, Intentional Space
The Pod’s design reinforces a restorative environment through guided reflection cards, finger labyrinths, and a QR code linking to guided meditations and calming music. Ambient backlighting and a fan provide gentle sensory cues and subtle white noise.

[2] Guided, Time-Aware Experience
Interior elements help staff manage short breaks without pressure. An hourglass and backlights that change color after 10 minutes cue users to the end of their session, while the main lights turn off when someone is inside to signal occupancy.

[3] Integration with Groundswell
The Pod fits within the hospital’s architecture and connects to the broader Groundswell system. A poem on the wall reinforces the program’s message, the nearby community art wall extends its sacredness, and the redesigned CTB email invites staff to engage with the space.

PLAYTESTING
Early participants expressed concern about “using the Pod correctly,” which revealed uncertainty around expectations
We ran multiple playtesting sessions to evaluate comfort, clarity, and usability. To address uncertainty, we refined instructional language and simplified tone to be more inviting. Follow-up sessions showed increased confidence and willingness to use the Pod.
IMPACT AND NEXT STEPS
Groundswell officially launched at UPMC Magee-Womens Hospital to an overwhelmingly positive response
On launch day, speeches were given, tears were shed, and hands rested on hearts. The project continues to serve as a living pilot within Women’s Cancer Services at UPMC Magee-Womens Hospital.

This prototype of Groundswell will be evaluated in a 12-month quality improvement study
In collaboration with UPMC, we are now collecting data to evaluate the Pod’s impact on staff well-being through the following metrics:

REFLECTIONS
Connecting My Healthcare Background
My own experience with emotional fatigue in healthcare helped me empathize with staff and build trust quickly, making co-design sessions more open and productive.
Letting Go of Perfectionism
Working with tight budgets, timelines, and workflows taught me to focus on feasible, high-impact solutions rather than perfect ones.
Collaboration & Coordination
I co-led cross-functional collaboration between hospital administrators, clinicians, designers, and fabricators, aligning timelines, budgets, and requirements to deliver a solution on schedule. This experience strengthened my ability to organize complex projects and keep diverse teams moving toward a shared goal.
ACKNOWLEDGEMENTS
Groundswell is a collaboration between Carnegie Mellon University School of Design; the University of Pittsburgh Schools of Medicine and Nursing, and the Gynecologic Oncology staff at Magee.
This project was made possible through the support of many individuals.
We are especially grateful to the Department of Obstetrics, Gynecology, and Reproductive Services and the incredible staff at Magee, who made this project possible. We also thank the College of Fine Arts at CMU; the UPMC Magee-Womens Hospital Medical Staff Fund; and the Paul D. Schurgot Foundation for their generous support.
Groundswell would not exist without an extraordinary community of artisans and donors. The restorative pod was made possible by NookPod’s gift of the structure; Greg Baltus from Hardware Assembly’s remarkable design, engineering, and fabrication skills; and components from Schlage, Density, Dixie&Grace, Z9 Machinings, and EHC Industries. Ryan Thompson made the walnut tabletop from wood donated by Eleanor Mackie Pigma. Catherine Liggett voiced meditations. Generous donations from Deborah Linhart, Pamela Meadowcroft, and Marge Petruska enabled us to distribute a set of restorative cards to every employee participating in this study—special thanks to Mark Baskinger for creative support and encouragement.
Shoutout to Carolyn Gavin for her wonderful artwork. Special thanks to Mark Staley, Kevin Lorenzi, and Michael Juan for donating their talents to help champion Groundswell.
We are grateful to Maggie Breslin (Patient Revolution), Stephanie Ciranni (CancerBridges), Dr. Adam Cowart, Pete Wendel, Christina Worsing, Craig Vogel, and Dr. Jenny Yu and Dria Barnes (Sixth House Advisory for Project Design OS) for their insights and feedback in the project’s early stages.
Thank you to my UPMC colleagues Dr. Sarah Taylor, Dr. Grace Campbell, Dr. Heidi Donovan, and Kendyll Grant.
Special thanks to Kristin Hughes, my mentor throughout the project, and to Lorin Anderberg, my collaborator and partner in bringing this project into UPMC. I am also grateful to Robertus Sucahyo and Kelly McDowell for their support in the early stages.
To everyone who contributed, thank you.